First aid for emergency conditions in pediatrics. Help for children in emergencies
Chapter 10. Emergency conditions in children
Allergic shock (anaphylactic shock)
Children react to various poorly tolerated factors to a much greater extent than adults. If a child comes into contact with such harmful substances, an allergic reaction occurs. It could be bee or wasp poison food products(most often cow's milk, chicken protein, fish, nuts), medications or allergens that enter the body through breathing (pollen, animal dander). With high sensitivity to these allergens, both local manifestations are possible, as we have already discussed, as well as general reactions of the body - up to shock with dysfunction of the respiratory and cardiovascular systems. This process is not associated with mental shock that occurs during significant emotional stress.
The clinical picture of shock is usually beyond doubt. The child's skin is pale and cold sweat appears. The pulse is frequent and difficult to detect. Breathing is frequent and shallow. Consciousness is confused, and loss of consciousness is possible in the future. With allergic shock, breathing difficulties (suffocation) associated with swelling of the mucous membrane of the respiratory tract, as well as swelling of the face and skin manifestations, are possible.
At the slightest suspicion of shock Call a doctor immediately!
Experience shows that most parents, who are aware of their children’s predisposition to allergic reactions, have at home, in agreement with the attending physician, the appropriate emergency medications that need to be used.
Until the ambulance arrived
In many cases, an excellent effect can be obtained from homeopathic medicines.
Apis mellifica D200, 1000 take 2 grains of whatever you have on hand; If necessary, you can repeat the reception. The drug is effective for allergic blisters and urticaria (urticaria) of any severity, as well as for swelling of the conjunctiva, eyelids, lips, and mouth.
Acidum carbolicum D200 is given to the child once - 2 grains. This is an adjuvant for anaphylactic shock with dysfunction of the cardiovascular and respiratory systems.
False croup
This is one of the special forms of laryngitis (inflammation of the larynx). The mucous membrane below the level of the vocal cords is inflamed and swollen, which significantly complicates the passage of air when the child breathes. Since in earlier times the name "croup" was associated with diphtheria, this disease, which has similar symptoms, is designated "false croup". The disease is usually associated with a viral infection, so it is most common during the cold season.
Sometimes, often unexpectedly and at night, a dry, barking, rough cough and wheezing when inhaling suddenly appear - signs of suffocation. This is the so-called false croup. This lack of breathing is expressed primarily in anxiety and a feeling of fear and can even lead to loss of consciousness. In children under one year of age, this disease is rare, since maternal immunity apparently plays a major role. Most often, false croup occurs in the second year of life, and boys are more often susceptible to this pathology than girls. As the child grows, the possibility of illness becomes less and less common. If you know that your child is prone to it, carry out preventive treatment in the fall, from the beginning of September. As one old pediatrician noted, foggy autumn provokes cough attacks.
Experience has long been accumulated in treating this process using natural means.
First aid for an acute attack
The most important thing for parents is to remain calm, not to lose their heads and try to calm the child, because the more scared he is, the worse he feels.
At the same time, you need to ensure a sufficient flow of fresh and cool air.
Try increasing the humidity in the room: place a wet towel on a hot radiator, turn it on in the bathroom hot water(steam should not be scalding); for repeated illnesses, it is better to purchase a special humidifier for a battery or device.
It is advisable to make a warm foot or general bath with a water temperature of 37–40 ° C, and you can add mustard to the foot bath (2 tablespoons per bucket of water). Mustard plasters can be placed on the chest, wrapping the child well.
Sometimes warm compresses on the neck and warm drinks help: milk with soda or Borjomi, fruit drinks, etc.
Doctors practicing anthroposophical methods actively use the simplest and effective remedy. Needs to be finely chopped onion, mix with a small amount of oil, heat this mass in a frying pan for so long until the onion becomes transparent (but do not fry!). Place everything on a cloth, cool until warm, cover the top with a thin cloth and place it on the larynx, and wrap a woolen scarf on top. Usually the attack goes away within 2-3 minutes. The same compress can be done prophylactically if you know that your child has already had attacks of false croup, you notice that the child has a cold, and you suspect that your baby may have an attack at night. In this case, it is better to make a compress at night.
Homeopathic medicines
In case of an acute attack of cough, give 5 grains every 5 minutes, in turn, the following drugs - Spongia D6, Rumex D6, Sambucus D6, Apis D6.
When improvement occurs, the intervals between taking medications are longer (10–20 minutes). You can place a hot chamomile infusion nearby for evaporation. Experience shows that in most cases such treatment can prevent the prescription of hormones (corticosteroids). In extreme situations, however, you should not give up suppositories with cortisone. If symptoms are dramatic, consult a doctor.
Anthroposophical preparations
Bryonia/Spongia comp. relieves an attack well if you give the remedy 3-5 grains every 10 minutes.
Larings D30 is a larynx organomedicine that allows you to relieve an attack instantly, so if your child is prone to such attacks, we recommend that you always have this drug at the ready during the cold season.
Autumn prevention of false croup
It is advisable to take 3 drugs: Spongia D12, Rumex D12, Aconite D12 - 5 grains of each drug once a day (in the morning - Spongia, in the afternoon - Rumex and in the evening - Aconite), the course is at least a month.
Convulsions
Seizures are a fairly common condition in children. There are many reasons for their occurrence: an increase in body temperature above 39.5 ° C, infection, acute poisoning, brain damage. During cramps, twitching may occur in the muscles and limbs, and in some cases, on the contrary, tension in the limbs develops with their maximum extension. During convulsions, the child seems to freeze with his head thrown back and his arms and legs frantically extended forward. This condition can last from a few seconds to 10 minutes or even longer. In some cases, convulsive twitching is observed only in certain muscle groups and may go unnoticed by parents. During an attack of convulsions, the child, as a rule, loses consciousness, the eyes close, the eyelids and other facial muscles twitching is possible, the teeth are tightly clenched. Sometimes foam appears on the lips. Involuntary urination often occurs. During an attack of generalized convulsions that lasts more than 2–3 minutes, the child’s lips may suddenly become bluish as breathing is temporarily interrupted and becomes convulsive.
Parents should know that any sudden loss of consciousness with convulsions that occurs for the first time requires immediate consultation with a doctor.
First aid before the doctor arrives
If your child suddenly begins to have seizures, try not to panic (although the sight of a child with seizures is indeed frightening), your child needs your composure at the moment. Take simple steps to ensure your child is not harmed during an attack.
First of all, without moving the child, turn him on his side so that he does not choke on saliva.
Make sure that there are no hard or sharp objects near his head that could hurt him during an attack.
Once you're sure there's nothing obstructing your baby's breathing, place a hard but not sharp object between your baby's teeth to prevent him from accidentally biting his tongue - this could be anything you have on hand, such as a folded leather glove (but not your finger!) or wallet.
After these activities, you can call your doctor.
After an attack, you need to transfer the child to the bed, free him from disturbing clothes and give him the opportunity to sleep.
After an attack, the child is drowsy, so you should not give him food or drink for 1–1.5 hours, so that due to drowsiness he cannot choke.
If a child has a high temperature, then even before the doctor arrives, you can begin to reduce it as indicated in the section on temperature.
If you stay in a stuffy room for a long time or stand in one place for a long time (during special events, etc.), the child may faint. In rare cases, this can happen with a sudden change in body position, such as getting out of bed quickly. Sometimes fainting can be caused by nervous tension, for example when taking a blood test.
Fainting occurs due to insufficient blood circulation to the brain, as a result of which the child loses consciousness and falls. Before this, he experiences unpleasant sensations, turns pale, the skin becomes covered with cold sweat, tinnitus and nausea occur. Most often, having fallen during a faint, a child quickly comes to his senses, since in a horizontal position the blood flows to the brain more intensely.
First aid
If they manage to support a child who has lost consciousness, he should still be put down. Raise your legs and lower your head to facilitate blood flow to the head. The window in the room must be opened to allow fresh air to enter. It is necessary to free the child from tight clothing, unfasten the buttons on the neck, and loosen the belt or strap. You can spray your face cold water, rub your temples with a cotton swab soaked in ammonia and let it smell.
In the hall, in a narrow passage between rows of chairs, they leave the unconscious person in place, in a sitting position, tilt the torso forward so that the head hangs as low as possible (due to compression of the abdomen, the blood flow rushes to the heart and head). The child should be allowed to remain in this position until he feels well again, but for at least 5 minutes.
Homeopathic medicines
Aconite D30 is given once 5 grains in case of fainting from fright.
Ipecac D6 is indicated, 3 grains every 10–15 minutes, if fainting is associated with disgust at the sight of blood.
Ipecac D6 or Carbo vegetabilis D6 is recommended in the above doses in case of significant heat or stuffiness.
Nux vomica D6 has a positive effect after mental fatigue; it is given 3-5 grains every 2 hours.
Sun and heat stroke
This condition is caused by overexposure to the sun's rays on your baby's uncovered head and neck. Prolonged stay without protection high temperature or in the sun, especially during physical exertion, leads to overheating of the head and brain and ends in sunstroke.
You should always think about making sure your child drinks plenty of juice (juices, water, or a mixture of both) on hot days. Make sure that your child, especially on vacation in warm countries, does not fall asleep in the sun. In extreme heat, especially with severe humidity, you should stay in the shade more. In summer, do not leave your child alone in a closed car, as the temperature in it often rises sharply.
Symptoms of sunstroke manifest themselves very vigorously: the head becomes hot, the face turns red, headaches appear, anxiety, dizziness, nausea to vomiting, a stunned state, and in the worst case, an unconscious state. If at the same time the body temperature rises sharply to 40 °C, then they speak of heat stroke. The condition worsens, loss of consciousness and convulsions are possible.
First aid
Sunstroke, especially severe cases of heatstroke, requires immediate medical attention. Before the doctor arrives, it is necessary to place the child in the shade, raising his head slightly, for example, placing him on the lap of the person accompanying him. Wet a cotton handkerchief with cold water, wring it out and place it on your head and forehead, wipe your body with a towel soaked in cold water. Repeat the procedure after 10 minutes.
Homeopathic medicines
Camphor D3 - as the first remedy, the drug should be given in 3-4 doses of 3 grains every 10 minutes, and then Cactus D3 in 2 doses after 10 minutes, and then repeat after 1-2 hours. You can give Camphor and Cactus at the same time using the “glass of water” method.
Aconite D3 and Belladonna D3 or Gelsemium D3 and Glonoin D3 are also very effective when used using the “glass of water method”.
Apis D6 is indicated for severe headaches and tension in the occipital region - 5 grains 3-4 times a day.
Natrium carbonicum D12-30 is useful when, after sunstroke, complaints of fever, headaches, dizziness, and inability to think when exposed to the sun reappear; accepted the same way.
In case of unstable blood circulation or loss of consciousness, call a doctor immediately.
Poisoning
If a toxic substance enters the body, it leads to poisoning, causing impairment and sometimes death. The most common causes of poisoning are medications, household chemicals (acetic acid, turpentine, soapstone solution, gasoline, household insecticides), poisonous plants and berries (wrestler, datura, henbane, wolfberry, hemlock, wild rosemary, marsh bogul, etc.), poisonous mushrooms, means for exterminating agricultural pests (herbicides), fertilizers, washing powders and other detergents, gas.
Most poisonings occur in younger children and before school age when, due to extreme curiosity, children, without thinking, take all sorts of objects into their mouths. The attractive packaging of liquids may lead them to believe that it is delicious lemonade. Naturally, poisoning can often be prevented, but, unfortunately, some parents understand this after the accident has already occurred.
Medicines and products household chemicals must be out of the reach of children!
The initial symptoms of poisoning can be severe nausea, vomiting, and abdominal pain. In case of poisoning chemicals the child may become lethargic, drowsy, indifferent, and in some cases the opposite picture is possible - extremely agitated. Possible loss of balance, convulsions, loss of consciousness.
Sometimes the child feels relatively well at first, but the condition may worsen gradually if the toxic substance is absorbed slowly from the stomach. Even 1-2 tablets of sleeping pills, antipyretic drugs or cardiac medications can cause severe, sometimes fatal poisoning.
First aid
In all cases, you should consult a doctor, even if the origin of the poisoning is known. If you find that the child has eaten (or drank) some medicines or chemicals, you must take the package (bottle) to the hospital so that doctors can select the necessary antidote.
The task of first aid for poisoning food is the fastest possible removal of poison from the body. To do this, you need to immediately do a gastric lavage. Give your child a large amount to drink warm water, then pick him up and tilt him over a basin or bucket and induce vomiting by pressing your finger or spoon on the root of his tongue. When washing again, you can add a 1% solution of baking soda to the water (1 teaspoon of soda per 0.5 liter of water).
In case of poisoning with corrosive substances (alkalis, acids) vomiting cannot be caused, because on the way back these fluids damage the esophagus again. In this case, immediately give plenty of fluids (water, tea) to dilute the toxic substance in the stomach.
Whatever the cause of poisoning - a chemical, plant, medicine or gas - the main task of parents is to immediately call an ambulance, since any measures taken before the ambulance arrives may be ineffective. And here the most logical and most expedient solution is hospitalization.
After eating poor quality food, effective remedies are recommended.
Homeopathic medicines
Nux vomica D6 perfectly helps with feelings of fullness in the stomach, bloating, nausea, vomiting, constipation.
Veratrum album D6 is useful for vomiting and diarrhea associated with the intake of poor quality products.
Hamomilla D6 relieves vomiting with abdominal pain.
Sepia D3 and Okoubaka D6 are effective against poisoning from poor-quality fish.
Pulsatilla D3 is given for poisoning due to consumption of fatty foods, pies, and pastries.
All these drugs can be given using the “glass of water” method.
Burns of the esophagus
This is a lesion of the mucous membrane of the organ, resulting from accidentally drinking a strong acid or alkali. This usually happens to curious young children who are attracted by unknown bottles. They may contain concentrated vinegar or hydrochloric acid, ammonia or a solution of potassium permanganate (potassium permanganate). The severity of the burn to the mouth, pharynx and esophagus depends on the amount of liquid swallowed. Since the burn causes severe pain, the child begins to scream loudly.
First aid
First of all, you need to quickly find out what the child has swallowed. Before the ambulance arrives, the child's face and mouth should be rinsed generously with cold water for several minutes. running water. You need to make sure that water does not flow into your eyes. You can rinse your child's mouth with a rubber bulb. To dilute the acid or alkali in the esophagus and stomach, you need to give the child a glass of cold water or milk to drink, but not more than the specified dose, so as not to cause vomiting. Often, due to the prevalence of the process, the child has to be hospitalized in the hospital.
I would like to remind parents about the rules for storing strong and toxic substances. After all, misfortune can happen to an adult if you don’t put things in order.
From the book Anesthesiology and Resuscitation: Lecture Notes authorLecture No. 5. Emergency conditions in pulmonology Acute respiratory failure is a pathological condition of the body in which the function of the external respiration apparatus is insufficient to provide the body with oxygen and adequate excretion
From the book Anesthesiology and Resuscitation: Lecture Notes author Marina Aleksandrovna KolesnikovaLecture No. 6. Emergency conditions in cardiology 1. Myocardial infarction Myocardial infarction is a discrepancy between the myocardial need for oxygen and its delivery, resulting in the formation of limited necrosis of the heart muscle. The most common reason– thrombus, less often –
author Arkady Lvovich Vertkin From book Ambulance. Guide for paramedics and nurses author Arkady Lvovich Vertkin From the book Ambulance. Guide for paramedics and nurses author Arkady Lvovich Vertkin From the book Ambulance. Guide for paramedics and nurses author Arkady Lvovich Vertkin From the book Ambulance. Guide for paramedics and nurses author Arkady Lvovich Vertkin From the book Nursing: A Guide author Alla Konstantinovna MyshkinaChapter 4 Emergency conditions Treatment measures for emergency conditions Anaphylactic shock Anaphylactic shock develops in response to the introduction of a foreign protein. All treatment measures are carried out promptly and comprehensively. To do this you should: 1) lay
author Elena Yurievna Khramova From the book Emergency Care Directory author Elena Yurievna Khramova From the book Emergency Care Directory author Elena Yurievna Khramova From the book Emergency Care Directory author Elena Yurievna Khramova From the book Emergency Care Directory author Elena Yurievna Khramova From the book Emergency Care Directory author Elena Yurievna Khramova From the book Emergency Care Directory author Elena Yurievna Khramova From book Complete guide symptoms. Self-diagnosis of diseases by Tamara RutskayaDoctor providing emergency assistance at the prehospital stage, based on the child’s age and the corresponding age-related anatomical and physiological characteristics, he must determine the specifics of the child’s emergency condition.
History is the most important component of emergency diagnosis at the prehospital stage. Unlike adults, young children are diagnosed in almost 50% of cases based on anamnesis and only in 30% based on the results of a physical examination.
Emergency conditions in children
What should doctors consider when diagnosing emergency conditions in children?
- Lack of constant monitoring of the patient.
- The possibility of developing a critical condition in children of the first year of life in the first minutes or hours after visiting a doctor against the background of a previously relatively satisfactory condition upon examination.
- Anatomical and physiological differences in the child’s body.
- Often low sanitary standards of the population.
This explains the priority of tactical overdiagnosis (“severification” of syndromes) during hospitalization of most patients in the first months of life.
The primary task of examining a child is to identify syndromes that determine the patient’s condition, and not the causes of the disease. When making a diagnosis, a media doctor, unlike doctors of most other specialties, must go from effect to cause.
How are medical emergencies diagnosed in children?
- The degree of impairment of vital functions and the need for emergency treatment measures according to vital indications are initially assessed;
- then the state of the central nervous system is determined (level of consciousness, presence of cerebral symptoms, convulsive syndrome), central hemodynamics, breathing, and, if necessary, emergency measures are taken.
The study of the functions of vital organs and systems, as well as the correction of their disorders in children and adults, have no fundamental differences.
If the state of the central nervous system, central hemodynamics and respiration are sufficiently stable, then the doctor begins a typical examination of the patient.
Given the limited time, the EMS doctor collects only the data necessary to develop the required tactical decision and the scope of emergency measures.
History of children when diagnosing emergency conditions
- change in child's behavior,
- physical inactivity, lethargy or hyperactivity,
- change in appetite
- sleep disturbance,
- drowsiness and lethargy in a usually active child - this may be a symptom of central nervous system depression,
- regurgitation, vomiting, one or two loose stools in young children do not necessarily indicate an infectious lesion of the gastrointestinal tract, this can be the beginning of any disease,
- the presence of previous perinatal pathology of the nervous system and its consequences to exclude the possibility of its manifestation,
- How did pregnancy and childbirth proceed?
- Is the child being seen by specialists?
- to clarify the possibility of the development of the disease against the background of an intrauterine infection, malnutrition, rickets, perinatal pathology, congenital malformations, etc.,
- information about vaccinations, post-vaccination reactions,
- contacts with infectious patients,
- allergy history.
Physical examination of children in an emergency is aimed at identifying threatening conditions.
The complexity of examining young children is due to the peculiarities of their anatomical, physiological, psychomotor and speech development. Thus, newborns experience a number of borderline conditions (physiological weight loss, jaundice, dyspepsia, etc.), have physiological tachycardia (120-140 per 1 min) and tachypnea (40-60 per 1 min), etc.
In children, it is necessary first of all to identify decompensation of breathing, blood circulation and the degree of damage to the central nervous system.
Breathing disorders in emergency conditions
- absence,
- bradypnoe,
- pathological type.
Circulatory disorders when diagnosing a patient’s condition
- disappearance of the pulse in the radial artery when blood pressure is below 50-60 mm Hg. Art.,
- disappearance of the pulse in the carotid artery when blood pressure is below 30 mm Hg. Art.,
- tachycardia,
- bradycardia,
- arrhythmia,
- "marbling" of the skin,
- cyanosis.
Emergency conditions for children - CNS examination
- the level of consciousness when verbal contact is impossible is determined by the child’s activity, by how he watches you and objects, whether he plays with a toy, how he screams or cries (a monotonous cry is characteristic of meningitis),
- diffuse cerebral reactions,
- convulsive syndrome (febrile seizures),
- nonspecific toxic encephalopathies (neurotoxicosis),
- the width of the pupils, their reaction to light,
- muscle tone, etc.
If meningitis is suspected, the doctor must remember that in children under 3 months of life, Kernig’s symptom is physiological, and Brudzinski’s symptoms are rarely detected, however, stiff neck muscles, hyperesthesia to all stimuli, elements of the “pointing dog” pose, a monotonous cry and light detectable symptom of “suspension”.
Help for children in emergencies
The sequence of actions of an emergency physician at the prehospital stage
Examination of the child:
- Establish contact with parents to collect anamnesis and ensure the patient’s calm state during examination.
- Get answers to questions:
- the reason for petition;
- circumstances of illness or injury;
- duration of the disease;
- time of deterioration of the child’s condition;
- means and medications used before the arrival of the ambulance doctor.
Development of a tactical solution(taking into account that decompensation of the condition occurs faster in children than in adults!):
If:
- the disease does not threaten the patient’s life;
- stable condition;
- The child’s material and living conditions are satisfactory and he is guaranteed necessary care, excluding a threat to his life - you can leave the child at home with the obligatory transfer of an active call to the clinic.
If:
- the nature and severity of the disease threatens the patient’s life;
- unfavorable prognosis of the disease;
- An unsatisfactory social environment and the age of the child suggest treatment only in a hospital setting - hospitalization of the child is necessary.
If parents refuse hospitalization, it is necessary to report this to the senior doctor at the EMS station and act on his instructions. Any refusal of examination, medical care, or hospitalization must be recorded in the EMS doctor’s call card and signed by the child’s parent or guardian. If the patient or parent (or guardian) of the child does not want to formalize the refusal of hospitalization in the form prescribed by law, then it is necessary to attract at least two witnesses and record the refusal. Now you know how to help children in emergency situations.
▲ Diagnosis of major emergency conditions.
▲ Urgent care for emergency conditions.
ASTHMATIC STATUS
This is a long-term persistent obstruction of the airways, in which bronchodilators that previously relieved an asthma attack do not have an effect. Unlike an attack of bronchial asthma, including a prolonged one, the leading role in the pathogenesis of status asthmaticus is played not by bronchospasm, but by edema, inflammation, dyskinesia of bronchioles, small bronchi filled with viscous, non-coughing sputum. The cessation of sputum drainage using natural mechanisms indicates the transition of a prolonged attack of bronchial asthma to asthmatic status. When the airways are obstructed by viscous, uncoughed sputum, swelling and inflammation of the bronchioles and small bronchi are associated, inhalation becomes difficult, and exhalation becomes active and prolonged. In these cases, when inhaling, the bronchi expand, allowing more air into the lungs than the patient can exhale through the narrowed bronchi filled with viscous mucus. He tries to intensify exhalation, strains pectoral muscles, which causes an increase in intrapleural pressure. In this case, the small bronchi are compressed, i.e., expiratory closure of the lower respiratory tract occurs, and then expiratory stenosis is added - prolapse of the membranous part of the trachea and main bronchi into the lumen of the respiratory tract during inhalation. The respiratory muscles perform enormous but ineffective work, consuming large amounts of oxygen. As a result, respiratory failure increases and hypoxia intensifies. Right ventricular failure gradually develops: the right ventricle has to overcome high intrathoracic pressure. Persistent obstruction of the airways with viscous sputum can be considered the first stage of status asthmaticus, right ventricular failure - the second, and metabolic disorders, expressed in hypoxia, respiratory and metabolic acidosis, hypohydration and adrenal insufficiency with all its consequences - the final one. The most important component respiratory failure in status asthmaticus is a violation of the drainage function of the respiratory tract, caused by hypersecretion and mainly a change in the consistency of sputum (it becomes viscous and is not removed using the natural mechanisms of lung cleansing).
Clinical picture. There are three stages of the asthmatic condition. The first stage is similar to a prolonged attack of suffocation. In this case, the patient becomes refractory to sympathomimetics, disturbances in the drainage function of the bronchi develop (sputum does not come out), and an attack of suffocation cannot be stopped for 12 hours or more. Despite the severity of the patient’s condition, changes in the blood gas composition remain insignificant: moderate hypoxemia (P0l 70-80 mm Hg) and hypercapnia (PCo2 45-50 mm Hg) are possible or, conversely, due to hyperventilation - hypocapnia (PCo2 less than 35 mm Hg) and respiratory alkalosis.
The asthmatic condition of stage II is characterized by progressive disorders of the drainage function of the bronchi, the lumen of which is filled with thick mucus. The “silent lung” syndrome gradually develops: the previously detected wheezing sounds are no longer heard over certain areas of the lungs. There are sharp disturbances in the gas composition of the blood with arterial hypoxemia (PCo2 50-60 mm Hg) and hypercapnia (PCo 60-80 mm Hg), mainly due to mixed acidosis. The patient's condition becomes extremely serious: consciousness is inhibited, the skin is cyanotic, covered with sticky sweat, severe tachycardia is noted, blood pressure tends to increase.
The asthmatic state of the third degree is characterized by significant dysfunction of the central nervous system with the development of a picture of hypercapnic and hypoxemic coma due to severe disturbances in the gas composition of the blood (PCo, more than 90 mm Hg, P0l less than 40 mm Hg).
Treatment. Intensive therapy is indicated: A restoration of airway patency (improving the rheological properties of sputum, lavage of the bronchial tree and elimination of expiratory stenosis); And reducing the harmful effects of hypoxia; And normalization of hemodynamics and correction of metabolism.
To liquefy sputum, aerosol inhalations of warm sterile water, isotonic sodium chloride solution, and 0.5-1% sodium bicarbonate solution are prescribed. Intravenous infusion of crystalloid solutions facilitates drainage of the respiratory tract. In addition, the goal of fluid therapy is to correct hypovolemia. Infusion therapy involves the administration of ringer lactate (12 ml/kg) during the first hour, then 5% glucose solution and isotonic sodium chloride solution in a ratio of 1:2 (100 ml/kg/day). To eliminate bronchospasm, high doses of aminophylline (20-40 mg/kg/day at a rate of at least 2 ml/h) are administered through a perfuser. The effectiveness of the drug is assessed by diuresis. Intravenous administration of glucocorticoids is indicated. They have a nonspecific anti-inflammatory effect, inhibit the production of antibodies, promote the release of mediators from mast cells, restore the response of beta-adrenergic receptors to catecholamines and relax the bronchial muscles. Preference is given to dexazone (initial dose 0.3-0.4 mg/kg, then 0.3 mg/kg). The intensive care complex also includes heparin (100-300 units/kg/day) and antiplatelet agents. Oxygen therapy begins with the supply of warm, humidified oxygen through a nasal catheter (oxygen concentration in the respiratory mixture 40%, gas flow 3-4 l/min). With an increase in Pco and severe initial hypercapnia, mechanical ventilation is indicated.
HYPOGLYCEMIC COMA
Hypoglycemic coma- an acute condition that develops with a rapid decrease in the concentration of sugar in arterial blood and a sharp drop in the utilization of glucose by brain tissue.
Etiology. This condition occurs in cases of insufficient intake of glucose into the blood or increased excretion from the body, as well as in cases of imbalance between these two processes. Observed in patients diabetes mellitus with an excess of administered insulin and inadequate intake of carbohydrate foods. A hypoglycemic symptom complex may develop in cases of using certain medicines(sugar-lowering sulfonamides), with a number of clinical syndromes accompanied by increased secretion of insulin (insulin-producing tumors). Unlike diabetic coma, hypoglycemic coma develops suddenly, loss of consciousness occurs in a matter of minutes.
Clinical picture. Characteristic signs: profuse sweat, pallor and wetness of the skin, wetness of the tongue, shallow rhythmic breathing, lack of acetone odor from the mouth and hypotonia of the eyeballs. Trismus of the jaws and a positive Babinski sign (on one or both sides) are possible. In addition, tachycardia, dullness of heart sounds, arrhythmia, lability of blood pressure, a sharp decrease in blood sugar, and the absence of sugar and acetone in the urine are noted.
Treatment should begin immediately: intravenously - concentrated glucose solutions (20%, 40%) without insulin (until the child shows signs of consciousness); inside - warm sweet tea, honey, jam, sweets, sweet semolina porridge, White bread(with mandatory monitoring of blood sugar).
DIABETIC COMA
Pathogenesis. Diabetic coma develops with the rapid progression of metabolic disorders as a result of late diagnosis of diabetes mellitus. The causes of coma in patients with diabetes may be a gross error in diet (eating food containing large amounts of sugar and fat), stopping the administration of insulin and other drugs that lower blood sugar, as well as inadequate doses. Exacerbation of diabetes mellitus is possible due to mental and physical trauma, stressful situations, infections, diseases of the gastrointestinal tract, when the intake, absorption and passage of food are disrupted, which leads to starvation of the body. In cases of increasing insulin deficiency, disturbances in the utilization of glucose by tissues, the processes of its oxidation and energy use by cells, and a decrease in the permeability of cell membranes to glucose are observed. The synthesis of glycogen in the liver is disrupted, and fatty degeneration develops. The breakdown of glycogen increases, and compensatory formation of glucose from proteins and fat occurs. Overproduction of the insulin antagonist - glucagon and counter-insular hormones (GH, ACTH, catecholamines), which have a fat-mobilizing effect, helps to increase the level of glucose in the blood to 28-40 mmol/l (500-700 mg%) or more. Hyperglycemia leads to an increase in osmotic pressure in the extracellular fluid, resulting in intracellular dehydration. Insulin deficiency leads to a sharp limitation of the body's ability to use glucose to cover its energy costs and stimulates the compensatory breakdown of fats, and to a lesser extent, proteins. Disruption of redox processes and intense protein breakdown in the liver lead to metabolic disorders, accompanied by the accumulation of ketone bodies, nitrogenous wastes and the development of uncompensated acidosis. Glucose, ketone bodies, and nitrogenous wastes begin to be excreted in the urine. The osmotic pressure in the lumen of the renal tubules increases and renal reabsorption decreases, which causes polyuria with a large loss of electrolytes - potassium, sodium, phosphorus, chlorine. Due to hypovolemia developing as a result of dehydration, severe hemodynamic disturbances occur (fall in blood pressure, decrease in stroke volume of the heart, decrease in glomerular filtration). Clinically, this is manifested by a collaptoid state and a decrease in urine output, up to anuria.
Clinical picture. Coma develops gradually over several hours or days. Fatigue, weakness, thirst, severe headaches, dizziness, ringing in the ears, agitation, insomnia, followed by lethargy, apathy and drowsiness, anorexia, nausea, vomiting, polyuria appear. Characterized by dry skin and mucous membranes, a dry tongue coated with a brown coating, the smell of acetone from the mouth, tachycardia, decreased blood pressure, muffled heart sounds, and sometimes arrhythmia. In diabetic coma, there are 4 stages of impaired consciousness: I - stunned (the patient is inhibited, consciousness is somewhat confused); II - drowsiness, somnolence (the patient falls asleep easily, but can independently answer questions in monosyllables); III - stupor (the patient is in a state of deep sleep and only comes out of it
Under the influence of strong stimuli); IV - coma itself (complete loss of consciousness, lack of response to stimuli).
Diabetic coma should be differentiated from uremic and hepatic coma. In diabetic coma, hyperglycemia and glycosuria, the smell of acetone from the mouth, and low blood pressure are pronounced; with uremic - the smell of urea, high levels of waste in the blood, a sharp increase in blood pressure; with hepatic - a specific smell (of liver) from the mouth, yellowness of the skin and mucous membranes, hemorrhages and scratching on the skin, enlargement and pain of the liver, dyspepsia, bilirubinemia, urobilin - and bilirubinuria.
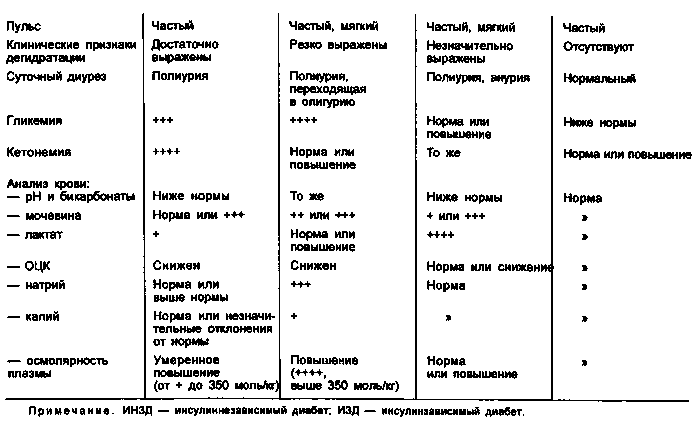
For differential diagnostic signs of comatose states developing in patients with diabetes mellitus, see table. 1.
Treatment is complex: administering insulin, combating acidosis and dehydration. Insulin therapy should be strictly individual. If the child has not previously received insulin, then this drug is administered to him at a dose of 1 U/kg. The first dose of insulin for preschool children is 15-20 units, for schoolchildren 20-30 units. If the child has previously received insulin therapy, he is prescribed at once the same daily dose that he received before the onset of coma. At the same time, to avoid hypoglycemia, a 5% glucose solution and an isotonic sodium chloride solution are infused intravenously in a 1:1 ratio. Repeated insulin injections are given in the first 6 hours at intervals of 1-2 hours (at the rate of 1 unit/kg). As the general condition improves, the intervals between injections increase. The total dose of insulin used to bring a child out of a coma, as a rule, does not exceed 150 IU/day, but sometimes it is higher. In the first days after a coma, insulin is administered 3-4 times a day under the control of blood and urine sugar levels, then the drug is administered twice a day. Infusion therapy carried out for the purpose of rehydration includes an isotonic sodium chloride solution in the first days, and Ringer's solution and a 5% glucose solution in a 1:1 ratio in the subsequent days. The total volume of administered fluid is determined at the rate of 100-150 ml/kg/day. Subsequently, the amount of glucose in the administered liquid is increased and potassium is added to it. In this case, for 1 unit of insulin there should be at least 1 g of dry glucose. When drawing up an infusion therapy program, the total amount of fluid is calculated based on the body’s needs and pathological losses. Antibiotics are prescribed to prevent secondary infection. After the child is brought out of a coma, enteral nutrition (physiological diet with limited fat) is indicated.
RESPIRATORY FAILURE
Etiology. The development of respiratory failure depends on many reasons, the main of which are disturbances in the central regulation of breathing, muscle activity of the respiratory complex apparatus and airway patency. Respiratory failure causes a change in the ratio of pulmonary ventilation and gas perfusion, which is very pronounced in lung diseases: bronchial asthma, emphysema, bronchiolitis, pneumonia, tumors, and developmental defects.
Violation of the central regulation of breathing occurs as a result of injury, cerebrovascular accident, edema and swelling of the brain of various etiologies, damage to the peripheral neuromuscular complex of both an infectious and toxic nature.
Impaired airway patency is observed with aspiration of amniotic fluid, stomach contents, obstruction of the airways by foreign bodies, swelling of the subglottic space of infectious, allergic and traumatic origin, congenital diseases, and developmental defects.
Clinical picture. One of the early signs is shortness of breath, often involving accessory muscles. The color of the skin is noteworthy. More often they are cyanotic, but their gray pallor, associated with microcirculation disorder and severe hypoxia, is more dangerous. Characterized by tachycardia or tachyarrhythmia, in more severe cases bradycardia. Due to respiratory failure, visceral functions are disrupted (decreased diuresis, sometimes intestinal paresis, acute erosions and ulcers in the digestive tract).
Treatment of respiratory failure: A immediate restoration of airway patency (if there is no injury to the cervical spine and neck, it is necessary to tilt the child’s head back as much as possible and place a cushion under his shoulders; to prevent the tongue from retracting, insert oral or nasal air ducts); And at the same time you need to actively suck out the contents from the upper respiratory tract, trachea under the control of a laryngoscope; And the most effective method of restoring the patency of the airways is bronchoscopy; nasotracheal intubation allows long-term maintenance of bronchial patency; And to improve the rheological properties of sputum and enhance the drainage function of the bronchial tree, aerosol inhalations of mucolytics and isotonic sodium chloride solution are used (it is better to use a sonic inhaler as a nebulizer); And oxygen therapy during spontaneous breathing is used under the control of P0i and the fractional concentration of oxygen in the respiratory tract.
Noah mixture (optimal oxygen concentration 40%). The concentration of oxygen in the gas mixture depends on the gas exchange function of the lungs and can fluctuate within wide limits even in the same patient during the day; And artificial pulmonary ventilation (ALV) helps eliminate hypercapnia, hypoxia, catecholemia, improve ventilation perfusion ratios, normalize pH, restore metabolic processes and microcirculation. Mechanical ventilation is carried out in an intensive care unit.
CIRCULATION DISORDERS
The cause of circulatory disorders can be cardiac or vascular failure, often a combination of both.
Vascular insufficiency Occurs when the relationship between circulating blood volume (CBV) and the capacity of the vascular bed changes. The main factors in the development of vascular insufficiency are a decrease in blood volume and impaired vasomotor innervation.
Clinical picture. Symptoms of acute vascular insufficiency: pale skin, cold sweat, narrowing of peripheral veins, a sharp decrease in blood pressure, frequent and shallow breathing. Vascular insufficiency manifests itself in the form of fainting, collapse and shock.
Goals of intensive care: A restoration of blood volume; And improvement of microcirculation; Elimination of acidosis and metabolic disorders; And in case of acute vascular insufficiency, the use of painkillers, antihistamines and sedatives, and oxygen therapy are indicated.
Acute heart failure in children(usually left ventricular) develops as a result of bacterial and toxic damage to the myocardium due to viral and bacterial infections, poisoning, rheumatic diseases, heart defects, acute renal failure and other endotoxicoses. Right ventricular failure occurs, as a rule, with long-term chronic processes in the lungs (bronchial asthma, chronic pneumonia, lung and heart defects, emphysema, spontaneous pneumothorax).
Clinical picture. The main symptoms: cyanosis of the skin, shortness of breath, expansion of the borders of the heart, tachycardia, dullness of heart sounds, pasty tissue, enlarged liver, dyspeptic disorders.
Goals of intensive care: A reduction of hypoxia and hypoxemia; And unloading of the small and large circle of blood circulation; And improvement of myocardial contractile function; And correction of electrolyte and metabolic disorders.
Inhalation of oxygen helps to increase its supply to tissues, reduce shortness of breath, tension of the respiratory muscles and vasoconstriction in the lungs. To reduce blood flow to the heart, diuretics (Lasix, furosemide) are used, for arterial hypertension - ganglion blockers (5% solution of pentamin), broncho- and antispasmodics (2.4% solution of aminophylline, papaverine, antianginal drugs and peripheral vasodilators (1 % nitroglycerin solution, 0.1% solution of perlinganite or isoket, naniprus), angiotensin-converting enzyme inhibitors (capoten and its derivatives), calcium antagonists (nifedipine), drugs with a positive inotropic effect (dopamine, dobutrex, dobutamine). To improve myocardial contractile function cardiac glycosides are used.The correction of metabolic disorders is carried out by administering 5% and 10% solutions of glucose, potassium and calcium salts, B vitamins, vitamin C. Trental is indicated among cardiovascular drugs.
syncope
Fainting (syncope)- an attack of short-term loss of consciousness, a type of vegetative-vascular crisis, manifested by an acute disturbance of cerebral blood flow. These attacks occur in children with an unstable autonomic nervous system (ANS), cardiac pathology, and more often in girls in puberty.
The etiology and pathogenesis of syncope (SS) have not yet been fully elucidated. It is impossible to exclude the role of “family” latent viruses with their vertical transmission from mothers to children, which simulates the hereditary nature of the disease. The pathogenesis of SS is dominated by constitutional dysfunction of the hypothalamus and limbic-reticular complex in the form of a violation of their release of neurotransmitters involved in the regulation of the autonomic functions of the body. However, discirculatory changes in the vertebral and carotid arteries and a number of cardiogenic causes may also be observed. In addition, children with SS exhibit delayed manifestations of perinatal encephalopathy (PEP) in the form of mild neurological signs of a residual organic nature, hypertensive-hydrocephalic syndrome, psychoemotional, motor, endocrine and vegetovisceral disorders. Inadequacy of the suprasegmental regulation of the ANS leads to the fact that such children remain vegetatively stigmatized throughout their lives and are extremely sensitive to external influences: mental trauma, painful stimuli, a sharp transition from a horizontal to a vertical position, overwork, intoxication. Occasionally, the causes of fainting can be a prolonged cough, urination, defecation, or sudden turns of the head. Autonomic disorders worsen during puberty, after infectious and somatic diseases. However, the role of intercurrent infections in the pathology of the ANS is extremely moderate and always secondary.
There are numerous classifications of SS, which is due to the lack of a generally accepted concept of pathogenesis. Despite the convention, all variants of SS can be divided into neurogenic and somatogenic (usually cardiogenic). Among the neurogenic ones, there are vasomotor, orthostatic, vagal, hyperventilation, cerebral, cough, hypoglycemic, nocturic, hysterical, associated with hypersensitivity of the carotid sinus, and mixed.
The clinical manifestations of all SS are stereotypical. In their development, three periods can be distinguished: the presyncope state, the fainting itself and the postsyncopal period. The period of precursors is characterized by a feeling of discomfort, lightheadedness, dizziness, tinnitus, blurred vision, lack of air, the appearance of cold sweat, “coma in the throat,” numbness of the tongue, lips, fingertips and lasts from 5 s to 2 minutes. Loss of consciousness is observed from 5 s to 1 min and is accompanied by pallor, decreased muscle tone, dilated pupils, and their weak reaction to light. Breathing is shallow, pulse is weak and labile, blood pressure is reduced. With deep fainting, tonic-clonic muscle twitching is possible, but pathological reflexes are absent. After fainting, the child orients himself quite correctly in space and time, but may be frightened by what happened, remains pale, adynamic, and complains of fatigue. He has rapid breathing, labile pulse, and low blood pressure.
Clinical picture. The most common variant of SS is Vasodepressor syncope, In which there is a sharp decrease in the peripheral resistance of muscle vessels and their dilatation, as well as a decrease in the volume of blood flowing to the heart, a decrease in blood pressure without a compensatory increase in heart rate (HR). In the pathogenesis of fainting, disruption of the cerebral mechanisms of regulation of the cardiovascular system and the lack of activation of the “muscle” pump play a role. Such SS most often occurs during prolonged standing in a stuffy room and is accompanied by many psychovegetative manifestations in the pre- and post-syncope periods. At Orthostatic syncope, On the contrary, there is an instant loss of consciousness without paroxysmal manifestations when moving from a horizontal to a vertical position due to a drop in blood pressure at a normal heart rate. In children of this group, there is a delay in the release of catecholamines and an increase in aldosterone secretion in response to an orthostatic factor. For Vagal syncope Bradycardia, asystole, a sharp drop in blood pressure, loss of muscle tone, and respiratory failure are characteristic, since the fields in the reticular formation (mesh formation) that regulate these systems are close to each other.
Excessive breathing, hyperventilation, leads to alkalosis, a decrease in PCo2 in the blood, suppression of the dissociation of oxyhemoglobin and multisystem changes in the body in the form of a prolonged presyncope, latent arrhythmias, paresthesia, myofascial disorders such as carpopedal spasm. When trying to stand up, repeated fainting is possible.
In patients with arterial hypertension, hypersensitivity of the carotid sinus is often detected. With pressure on the carotid sinus, turning the head, during eating, vagal, vasodepressor or Cerebral Options SS. The latter option is based on a sharp deterioration in blood supply to the brain with satisfactory hemodynamic parameters. The presyncope period may be absent, loss of consciousness is accompanied by loss of muscle tone, a feeling of severe weakness due to increased sensitivity not only of the carotid node, but also of the boulevard centers. The post-attack period is characterized by asthenia, a feeling of unhappiness, and depression.
A coughing attack can lead to a sharp increase in intrathoracic and intra-abdominal pressure, swelling of the neck veins, and cyanosis of the face. With dysfunction of the central brainstem formations responsible for the regulation of breathing, vasodepressor and cardioinhibitory reactions and a drop in cardiac output as a result of stimulation of the receptor system of the vagus nerve are possible. Similar mechanisms of SS are observed when the trigger zones of the glossopharyngeal and vagus nerves are irritated during chewing, swallowing, speech, urination and defecation.
Hypoglycemic syncope They are observed when the concentration of sugar in the blood decreases to 2 mmol/l or more (reaction to hyper-insulinemia), brain hypoxia, as a result of which the child experiences drowsiness and disorientation, gradually turning into a coma. Autonomic disorders are also characteristic: sudden sweating, internal trembling, chill-like hyperkinesis (hyperadrenalemia). When drinking sweet tea, all symptoms disappear instantly. Syncope of hysterical nature They arise in a conflict situation and the presence of spectators, are demonstrative in nature and are often a way of self-expression in neuropathic children. For young children (up to 3 years old) Fainting with respiratory arrest. They always begin with crying, then the child stops breathing and cyanosis appears. In this case, the limbs are rigidly extended, convulsive movements are possible, after which relaxation and breathing restoration occur. At older ages, such children experience vasovagal SS. In young children, after head injuries, it is possible Pale type of fainting. At the same time, the child begins to cry, then suddenly turns pale, stops breathing, and develops muscle hypotension. This condition quickly normalizes. Such attacks are also associated with increased vagus nerve reflexes. EEG is normal, which helps rule out epilepsy.
Cardiogenic syncope They occur as a result of a drop in cardiac output below the critical level required for effective blood flow in the vessels of the brain.
The most common causes of cardiogenic CV are heart diseases that lead to the formation of mechanical obstructions to blood flow (aortic stenosis, pulmonary hypertension with pulmonary artery stenosis, tetralogy of Fallot, atrial myxoma, cardiac tamponade) or rhythm disturbances.
Heart rhythm disturbances (primarily brady- or tachyarrhythmia) are a common cause of CVD. In case of bradycardia, it is necessary to exclude the presence of sick sinus syndrome in the child, which occurs due to organic damage to the atrial myocardium. Sinus node dysfunction is manifested by bradycardia less than 50 per minute and periods of absence of waves on the ECG - asystole. Classic example CV of arrhythmic origin is Morgagni syndrome-Adams-Stokes, Characterized by the occurrence of attacks of sudden loss of consciousness, convulsions, pallor followed by cyanosis, and breathing problems. During an attack, blood pressure is not determined and heart sounds are not heard. Periods of asystole can last 5-10 s. Often such attacks occur during the transition from partial atrioventricular block to complete. Fainting occurs less frequently when the interval lengthens Q-T, Wolf-Parkinson-White syndrome, paroxysmal tachycardia, group extrasystoles. The following factors are of great diagnostic importance: the presence of a cardiac history, a feeling of interruptions in the heart area before the onset of fainting, the connection between a sudden loss of consciousness without warning signs and physical activity, ECG data. The prognosis for this type of SS is worse than for neurogenic syncope. Cardiogenic SS is differentiated from various manifestations of epilepsy. In this case, the role of the orthostatic factor, changes in hemodynamic parameters, and the absence of epilepsy-specific changes in the EEG are taken into account.
Emergency care and treatment for syncope:
And during an attack, you should put the child in a horizontal position, loosen the tight collar, give him hot sweet tea and provide access to fresh air; Or you can reflexively influence the respiratory and cardiovascular centers (inhalation of vapors ammonia or spraying the patient with cold water); And with a prolonged course, injections of adrenaline or caffeine are indicated; And in the interictal period, it is necessary to carry out physical hardening, resistance training to the orthostatic factor, and psychotherapy. The child should be taught breathing control techniques and getting out of bed slowly. Gymnastics, skiing, running, various water procedures, exercise therapy, massage are useful;
A course of restorative therapy, taking into account the predominance of one or another autonomic tone in the child. For vagotonia, ascorutin, vitamins B6 and B|5, calcium preparations, tonics, nootropil, vegetotropic drugs (belloid, etc.) are used. In case of sympathicotonia, vitamins B, B5, PP, potassium preparations, mild sedatives and beta-blockers (obzidan) are prescribed. Antiarrhythmic drugs are often used for cardiogenic syncope.
ACUTE LIVER FAILURE
Acute liver failure is characterized by the development of a severe general condition of the child with a sharp impairment of all liver functions due to necrosis of its cells.
Etiology. Causes of acute liver failure: And liver diseases (acute and chronic hepatitis, cirrhosis,
Neoplasms, alveolococcosis, etc.); And obstruction of the biliary tract and acute cholangitis; And diseases of other organs and systems (heart and blood vessels, connective tissue, infections); And poisoning with hepatotropic toxic substances, poisonous
Mushrooms, medications; And extreme effects on the body (trauma, surgery, burns, purulent-septic process, disseminated intravascular coagulation syndrome, portal vein thrombosis).
Clinical picture. Among the clinical symptoms, attention is drawn to icteric staining of the skin and mucous membranes, an increase in signs of hemorrhagic syndrome, a characteristic “liver” odor from the mouth, ascites, hepatospleno-megaly, neuropsychic disorders, the severity of which determines the degree of hepatic coma. In grade I, confusion, euphoria, sometimes depression, mental retardation, disorientation, and tremor are noted; in degree II (precoma) - confusion, severe drowsiness, behavioral disorders; with III (stupor) - almost continuous sleep, sometimes agitation, severe confusion, disorientation, tremor; IV degree (coma) is characterized by loss of consciousness, lack of response to painful stimuli, and muscle atony.
Intensive therapy: A limitation or cessation (in coma) of protein intake and
Table salt; And parenteral nutrition is the administration of 10% and 20% glucose solutions (120-150 ml/kg body weight) with the addition of insulin (at the rate of 1 unit per 1 g of dry glucose); And intravenous administration of a 10% solution of glutamic acid from 2 to 10 ml daily for 20 days and a 10% solution of calcium chloride in age-related doses;
And high cleansing enemas, the prescription of laxatives (to reduce the absorption of protein and its breakdown products into the blood);
And the introduction through a tube of broad-spectrum antibiotics, metronidazole, enterosorbents, cimetidine, lactulose; administration of antioxidants, unithiol, antihypoxants, corticosteroids (intravenously, in large doses - from 7 to 20 mcg/kg/day based on prednisolone), vitamins A, group B, C, K, riboxin, methionine, contrical, luminal;
A powerful hepatotropic effect is exerted by intravenous administration of 1 mg of glucagon in combination with 10 units of insulin in a 5% glucose solution, as well as L-dopa in large doses and solcoseryl with a 5% glucose solution;
And hemo- and plasma transfusions, 20% albumin solution;
And hemosorption, plasmapheresis and hemodialysis are for removing toxins;
And the use of anabolic hormones (Nerobol, Retabolil) to improve metabolic processes in the liver.
ACUTE RENAL FAILURE
Acute renal failure (ARF) is characterized by impaired renal function with the development of azotemia, uremia, electrolyte, acid-base and volumetric disorders.
surge arrester may be Prerenal(with a decrease in blood volume, arterial hypertension, severe heart failure, liver failure), Renal(with acute tubular necrosis after prolonged ischemia or exposure to nephrotoxic substances, with damage to arterioles in cases of malignant arterial hypertension, vasculitis, microangiopathies; with glomerulonephritis, acute interstitial nephritis, metabolic disorders with intrarenal deposits) and Postrenal(for obstruction of the ureters and lower urinary tract).
The main objectives of therapy: Providing forced diuresis for the purpose of dehydration,
Reducing uremic intoxication and hyperkalemia; And dehydration, aimed at quickly eliminating extracellular fluid (administration of diuretics, in particular Lasik-sa - up to 12 mg/kg/day). In case of overhydration, accompanied by a sharp drop in potassium excretion and the development of hyperkalemia, it is advisable to induce artificial diarrhea with sorbitol (a 70% solution is administered orally in a dose of up to 250 ml); And to reduce the negative effect of excess potassium on the myocardium, intravenous administration of a 10% calcium gluconate solution at a dose of 0.5 ml/kg in combination with a hypertonic glucose solution is necessary.
Indications for hemodialysis:
▲ lack of positive dynamics when administering large doses of diuretics (over 12 mg/kg body weight);
▲ hyperkalemia (potassium content in the blood serum over 6 mmol/l), metabolic acidosis (BE over 12 mmol/l), increased urea content in the blood (21-25 mmol/l, its daily increase is more than 3-5 mmol/l) ;
▲ overhydration with an increase of more than 7% of body weight, pulmonary and cerebral edema.
In the fight against uremic intoxication and acidosis, they also use conservative methods extrahepatic blood purification: siphon enemas (morning and evening) with the addition of 2% sodium bicarbonate solution, gastric lavage and skin toilet. In order to slow down the increase in azotemia, provide the body's basic need for calories and reduce catabolic processes in the body, patients are prescribed fractional meals (every 3-4 hours) with a sharp limitation of the protein content in food. For arterial hypertension, which often accompanies acute renal failure, the drugs of choice are angiotensin-converting enzyme inhibitors. The most effective use of captopril is in a daily dose of 1-8 mg/kg (administered at intervals of 6 hours). Calcium antagonists (nifedipine) can also be used.
BRAIN SWELLING
Brain swelling- severe syndrome of nonspecific damage to the central nervous system, developing in infectious and somatic diseases, acute neuroinfections, epistatus, cerebrovascular accident, and skull injuries.
Clinical picture. The main symptoms: headache, vomiting, impaired consciousness (from mild depression to deep coma) indicate intracranial hypertension. One of the manifestations of cerebral edema may be convulsive syndrome.
Objectives of intensive care for cerebral edema:
▲ elimination of the underlying disease; And dehydration.
For the purpose of dehydration, hypertonic solutions are used intravenously (10% and 20% glucose solutions, 25% magnesium sulfate solution), colloidal solutions (reogluman, reopoliglucin, reomak-rodex at the rate of 10 ml/kg/day), mannitol, mannitol (0.25 -0.5 g of dry matter per 1 kg of body weight per day), as well as diuretics (Lasix - 1-4 mg/kg/day, aminophylline - from 6 to 8 mg/kg/day). To increase osmotic pressure, albumin and plasma are administered, in order to improve microcirculation and brain metabolism - veno-ruton (6-8 mg/kg/day), cavinton (0.5-0.6 mg/kg/day), trental (3 - 4 mg/kg/day), nootropil (100-160 mg/kg/day), glutamic acid (10-12 mg/kg/day intravenously). The administration of dexazone (0.2-0.4 mg/kg/day) and contrical (300-600 units/kg/day) is indicated.
For convulsive syndrome - correction and maintenance
Vital functions of the body, anticonvulsants
And dehydration measures. It is necessary to provide:
And free airway patency;
And oxygen therapy, if mechanical ventilation is indicated;
And stabilization of hemodynamics;
And monitoring the state of single-electrolyte metabolism, acid-base balance (ABC), biochemical indicators of homeostasis. If any of these violations are present,
Their immediate correction.
Anticonvulsant therapy:
And intramuscular or intravenous administration of a 2% hexenal solution or a 1% sodium thiopental solution (2-5 ml) until the seizures stop. If seizures return, these drugs can be re-administered. Seduxen, Relanium, and 20% sodium hydroxybutyrate solution have a good anticonvulsant effect;
And for the purpose of dehydration, diuretics (Lasix), a 25% solution of magnesium sulfate (at the rate of 1 ml per year of the child’s life), and concentrated solutions of glucose are administered.
CONVASIONS
Convulsions are sudden attacks of clonic or clonic-tonic involuntary muscle contractions with or without loss of consciousness.
There are general cramps and cramps of individual muscle groups. A special type of them are epileptic seizures.
Etiology. Convulsions occur due to organic or functional damage to the nervous system. Seizures of organic origin can be caused by inflammatory, mechanical or vascular disorders, as well as the presence of a space-occupying lesion in the brain. Convulsions of functional origin occur due to metabolic disorders (hypoglycemia, hypocalcemia, hypochloremia, etc.), transient vascular disorders, exposure to toxic or physical factors of a temporary nature. There are tonic, clonic, mixed - clonic-tonic, tetanic convulsions.
Clinical picture. Regardless of the etiology, seizures are characterized by a sudden onset, motor agitation, impaired consciousness and loss of contact with the outside world. In this case, the head is thrown back, the arms are bent at the elbow joints, the legs are extended, tongue biting, a slowdown in the pulse, and a decrease or short-term cessation of breathing are often observed. Such a tonic convulsion lasts no more than 1 minute and is replaced by a deep breath and restoration of consciousness. A clonic spasm begins with twitching of the facial muscles with pe-
Going to the limbs. Then noisy breathing, foam on the lips, tongue biting, and increased heart rate appear. Convulsions can be of varying duration and follow one after another; sometimes result in death. After an attack, the child falls asleep, and when waking up, he may not remember anything and feel healthy. Tetanic spasms are muscle contractions that follow each other without relaxation and are accompanied by pain. To determine the cause of convulsive attacks, it is necessary to collect a detailed history, conduct a thorough neurological and somatic examination, functional studies, blood, urine, and cerebrospinal fluid tests.
Seizures in children aged 1-6 months
The appearance of seizures in newborns and infants is due to their tendency to generalized reactions due to the high permeability of the blood-brain barrier and blood vessels, metabolic lability and sensitivity of nervous tissue to various agents. Seizures may be caused by Anomalies in the development of the brain and skull. In this case, seizures appear during the newborn period, are more often tonic and are caused by defects of the brain (macro-, micro- and anencephaly) or skull bones (internal hyperostosis). To clarify the diagnosis, cranio- and pneumoencephalography are used, and the karyotype (genetic damage) is determined.
Convulsions Infectious (inflammatory) genesis Caused primarily by viral infections (rubella viruses, herpes simplex viruses, cytomegaloviruses - CMV). Brain damage due to rubella is often combined with congenital heart defects, congenital cataracts, deafness, and neurological retardation. mental development, later with dental anomalies, etc. CMV brain damage develops simultaneously with jaundice and hepatic coma. CMV is detected in urine, saliva, and puncture organ material. The herpes virus causes severe necrotizing encephalitis or meningoencephalitis, hepatitis with jaundice and hemorrhages. Bacterial infections are most often transmitted to the fetus not in utero, but intranatally (the cause of seizures in this case is purulent meningitis or hyperthermia). Congenital toxoplasmosis Often accompanied by macrocephaly, microphthalmia, the formation of intracranial calcifications (usually in the region of the subcortical nuclei), pigmented chorioretinitis and atrophy of the optic nerves with loss of vision. If a congenital infection is suspected, bacteriological and virological studies should always be carried out simultaneously in the child and mother.
Seizures in newborns may be due to Immaturity, asphyxia Or Brain hemorrhages. Immature and premature babies often experience twitching of the limbs, rigidity,
Conjugation of eyeballs; in full-term infants - unilateral convulsions, drowsiness. Hemorrhages in the fundus and blood-stained cerebrospinal fluid may indicate massive hemorrhage and hypoxic brain damage.
Tetanus In newborns and infants, it is characterized by a typical clinical picture - total tonic convulsions (opisthotonus) and trismus of the masticatory muscles. Currently observed very rarely.
Metabolic cramps Often caused by a violation of the water-electrolyte balance during exicosis and rehydration. Thus, with inaccurately balanced infusion therapy (hyper- or hyponatremia), severe seizures with subsequent neurological disorders are possible. The causes of seizures can be hypoglycemia (with intrauterine degeneration of the fetus or in a child whose mother suffers from diabetes), hypocalcemia (with rickets, hypoparathyroidism and pseudohypoparathyroidism), hypomagnesemia (congenital, with poor or poor nutrition, malabsorption syndrome). For differential diagnosis, biochemical tests of blood and urine are performed, and the content of hormones in plasma is determined. The absence of acute phase indicators of inflammation confirms the possible metabolic nature of the disorders.
Iatrogenic seizures Associated with taking high doses of medications and/or with poor (slow) release of them from the body (caffeine, penicillin, etc.).
Amino acid metabolism disorder(phenylketonuria, histidinemia, maple syrup disease, homocystinuria, tyrosinosis, etc.) is diagnosed by chromatographic examination of urine and serum. In this case, mental and motor development delays and convulsions are often observed.
Seizures in children older than 6 months
In children of this age, the development of non-epileptic seizures should first be excluded.
Febrile seizures(under the age of 3 years) often occur before an increase in body temperature or at the height of a febrile reaction. They usually do not occur in children under 6 months and older than 4 years. Frequent attacks of seizures (more than 3 times a day), focal or predominantly unilateral seizures, subsequent development of paresis and the presence of pathology on the EEG indicate the impossibility of febrile seizures. In this case, a lumbar puncture should be performed to rule out meningitis and encephalitis.
Brain hemorrhage Or vascular disorders may cause the appearance of sudden unilateral and then generalized convulsions with fever, impaired consciousness and subsequent paralysis. Their immediate causes may be anev-
Rhysms, embolism of the middle cerebral arteries or their branches, venous thrombosis, abscesses, thrombocytopenic purpura, systemic lupus erythematosus (SLE), systemic vasculitis, sometimes fibromuscular hyperplasia of the cerebral arteries, diagnosed by repeat angiography. Eclamptic or pseudouremic Convulsions Can be The initial symptom of acute nephritis(an increase in blood pressure is important in diagnosis).
Syncopal seizures- short-term loss of consciousness with short generalized tonic-clonic convulsions (vagovasal reflex reactions with vasomotor collapse) are not uncommon in children over 4 years of age and especially during puberty. To establish a diagnosis, it is important to measure blood pressure (low), identify arrhythmia or paroxysmal tachycardia, and the presence of a previous stressful situation.
Brain tumors They can provoke both focal and generalized seizures, most often when they are localized in the posterior cranial fossa of the brain. Tumors grow slowly, and short-term cramps may be the only symptom of the disease for a long time. In these cases, it is very important to conduct a diagnostic search: EEG, angiography, scintigraphy, computed tomography and magnetic resonance imaging. The cause of seizures may be pseudotumor cerebri. This is a peculiar condition caused by restriction of venous blood flow in otitis media with sinus thrombosis, limited encephalitis or adhesive arachnoiditis. The diagnosis can be confirmed by a thorough examination of the patient and dynamic monitoring of him.
Among the rarer causes of seizures are Tuberous sclerosis(pseudotumoral nodular growths in the brain with glycogen accumulation). Convulsions in this pathology are generalized, clonic-tonic. The child is lagging behind in mental development. The diagnosis is confirmed by the presence of intracranial areas of calcification, tumor-like formations in the retina and brownish papular rashes on the skin of the face.
Brain abscesses Sometimes they manifest as convulsions without inflammatory laboratory signs (decreased ESR, slight leukocytosis) and increased intracranial pressure.
Hitting the brain With blood flow Ascaris larvae, Finn pig Or Canine tapeworm Causes seizures, often in combination with a violation of cranial innervation, ataxia, aphasia, meningism, hydrocephalus, and psychotic behavior. Detection of calcified areas in the brain, protein and eosinophilia in the cerebrospinal fluid, eosinophilia in the blood and antibodies in the serum allows us to clarify the diagnosis of helminthiasis.
Convulsions of infectious (bacterial) origin In children of any age, they are most often caused by coccal flora. Meningococcal meningitis is manifested not only by convulsions, but also by fever, vomiting, hyperesthesia, tension of the large fontanel or its bulging (in children of the first year of life) and typical hepatitis.
Morragic star-shaped rash. In other coccal infections, meningitis is combined with sore throat, pneumonia, otitis, peritonitis, etc. In differential diagnosis, it is important to take into account changes in the cerebrospinal fluid (number and type of cells, concentration of protein, sugar, chlorides, presence and type of microbe). Candidiasis meningitis is very rare and is usually diagnosed in cases of generalized candidiasis.
The causes of seizures in both younger and older children can be Copper metabolism disorders AND Decreased ceruloplasmin content in blood plasma(Konovalov-Wilson and Menke diseases). With Konovalov-Wilson disease, hyperpigmentation of the cornea (Kaiser-Fleischner rings) in combination with liver pathology is observed; with Menke disease, hypothermia, fragility and thinning of hair, dementia, rickets-like bone changes, elongation and tortuosity of the arteries (with angiography).
In etiologically unclear cases of seizures in combination with delayed psychomotor development, one should always exclude the presence of metabolic disorders in patients, first of all, disorders of amino acid metabolism, then protein, fat and carbohydrate metabolism.
Psychogenic seizures They are divided into respiratory, hysterical and hyperventilation. Respiratory spasms occur in children 1–4 years of age after minor injury or infection. At the same time, the child screams and has a respiratory pause, accompanied by cyanosis and twitching (until breathing is restored). In other cases, the child screams continuously, without breathing, until deep cyanosis (“rolls over”). Muscle hypertonicity appears, up to opisthotonus and clonic-tonic convulsions. Their reason is hypoxia against the background of affect. EEG is practically unchanged, especially outside of an attack.
Hysterical fits Occurs in school-age children and usually mimics seizures. The frequency of twitching is less than with true clonic convulsions, and tonic convulsions are worm-like in nature. In addition, there are no typical signs of autonomic disorders (sweating pale face, drooling, involuntary urination at the end of a seizure, tongue biting, etc.). EEG - no changes.
Hyperventilation tetany It is more often observed in children during puberty, caused by an effort of will or fear, combined with palpitations, paresthesia, and respiratory alkalosis. The attack is relieved by breathing into a plastic bag without access to air. Sometimes hyperventilation convulsions are observed with brainstem encephalitis.
Epileptic convulsions They are observed at different ages: infancy, preschool, school, puberty and differ in clinical manifestations and typical EEG changes. There are idiopathic (genuine, unknown etiology) and residual (due to brain damage in early childhood,
Kernicterus, trauma, hemorrhage, congenital anomalies, inflammation) epilepsy. In most cases, confirmation of the diagnosis is possible with dynamic clinical observation and repeated EEG studies.
Epileptic seizures
There are propulsive minor, major and focal epileptic seizures.
Propulsive petit mal seizures Develops in infants. They are characterized by repeated flexion movements of the torso and head with throwing up the arms and bending the legs. Lightning-fast convulsions (lasting several seconds) with loss of consciousness are possible, repeated throughout the day, especially after waking up. In these cases, the EEG reveals mixed diffuse convulsive activity. At preschool age there are Myoclonic jerks With acute loss of muscle tone, rapid falls, attacks of nodding, blinking and screaming, as well as “absence seizures” - shutdowns. Their duration is 1-2 s. In this case, twilight states often occur, and later - delayed psychomotor development. The EEG shows generalized bilateral synchronous irregular peaks, as well as sharp and slow waves.
At school age, the manifestations of minor attacks are different: loss of consciousness, half-open eyes, swallowing, licking, chewing or tugging movements, rhythmic twitching of the muscles of the face and hands for 5-30 seconds - most often in the morning or when tired; EEG shows generalized flashes of bilateral peaks and waves.
At puberty, symmetrical myoclonic seizures with throwing up of the arms are observed without loss of consciousness, more often upon awakening, lack of sleep. They can be isolated or in the form of volleys and last several seconds or minutes.
Grand mal seizures epilepsy Possible at any age. A major seizure in 10% of cases is preceded by an aura (premonitory period). Then the child falls screaming, he has a tonic convulsion lasting up to 30 seconds with opisthotonus, apnea, cyanosis and transition to clonic convulsions lasting up to 2 minutes, with salivation, sometimes vomiting, involuntary urination, defecation and subsequent falling asleep. The seizure may occur during sleep or before awakening, and is sometimes combined with psychomotor or focal seizures. The EEG shows general changes and peaked waves at rest (provoked by hyperventilation or insomnia).
Focal seizures (Jackson's epilepsy) Characterized by an aura, localized clonic twitching, sometimes transient partial paresis; lasts seconds, minutes or hours. The EEG shows focal or multifocal foci of convulsive activity with provocation by sleep. In most cases, Jacksonian epilepsy is the result of previous trauma, inflammation or hemorrhage in the brain, often in the neonatal period.
Shock
Shock is a syndrome characterized by severe disorders of central and peripheral circulation, respiration, metabolism, all types of metabolism, and depression of the central nervous system.
In pediatric practice, the most frequently observed the following types shock:
▲ hemorrhagic or hypovolemic - with massive blood loss or severe dehydration of the body;
▲ traumatic - in case of severe injury, surgical interventions, defeat electric shock, burns, sudden cooling, compression of the body;
▲ toxic-septic - for severe infectious and septic processes;
▲ anaphylactic - as a result of allergic reactions during the administration of drugs, vaccines, serums, transfusion of protein drugs, etc.
Clinical picture. There are 3 phases of shock: erectile, torpid and terminal. In the first phase, due to an excessive flow of impulses from the pathological focus, generalized excitation of the nervous system occurs. Clinically, this is manifested by increased motor activity, shortness of breath, tachycardia, and increased blood pressure. The second phase of shock is characterized by deep inhibition of the nervous system due to its overexcitation in the first phase. A disorder of nervous regulation causes severe disturbances in blood circulation, respiration, and the functions of the endocrine system, primarily the adrenal glands. The immediate cause of a threat to the life of a patient in shock is disturbances in hemodynamics and gas exchange. In the torpid phase, hypotension quickly increases and BCC decreases (by 25-40% in hemorrhagic or hypovolemic shock), centralization of blood circulation occurs, caused by spasm of the capillary network. With the further development of the shock state, gas exchange disturbances are aggravated due to changes in the volume of blood volume, microcirculation disorders, depression of the respiratory center, and hypofunction of the adrenal glands. As a result of these disorders, renal blood flow decreases, up to acute renal failure. Shock is necessarily accompanied by disseminated intravascular coagulation syndrome, and often by convulsions (due to cerebral edema).
Treatment. The goal is to maintain hemodynamics with the help of intravenous fluid infusions, vasopressors, agents with a positive inotropic effect (dopamine, dobutrex) and corticosteroids. Intensive therapy begins with rapid replenishment of blood volume through the administration of saline, colloidal solutions and blood products. If necessary, emergency correction of blood clotting and electrolyte balance disorders is carried out. The use of adrenaline and dopamine is indicated. If there is no danger of bleeding, heparin (100-300 IU/kg/day), as well as inhibitors of the kallikrein-kinin system (Gordox, Contrical, Trasylol), should be used. For detoxification and improvement of microcirculation, low molecular weight dextrans (reopolyglucin, hemodez) are used. In traumatic shock, the triggering mechanism for microcirculation disruption is the flow of pain impulses. Analgesia and blockade of pain impulses prevent spasms in the microcirculation system. Infusion therapy, taking into account the replenishment of the deficit of bcc and improvement of the rheological properties of blood, is similar to that carried out for hemorrhagic shock.
Burn shock Develops as a result of extremely strong painful irritation emanating from an extensive wound surface and toxemia. Feature clinical picture burn shock is a more pronounced and prolonged erectile phase. In this case, the torpid phase is characterized by acute renal failure. The general principles of therapy are almost the same as those outlined above. Particular attention should be paid to the treatment of renal failure.
Toxic-septic shock Characterized by the development of acute cardiovascular failure due to intoxication caused by the septic process. Clinically manifested by a sudden deterioration of the condition, first hyper- and then hypothermia, a drop in blood pressure, and severe microcirculation disorders. Consciousness is confused, up to the development of coma. Signs of acute renal failure (ARF) are increasing. Features of therapy include intravenous administration of broad-spectrum antibiotics, the use of hyperimmune drugs, and large doses of corticosteroids.
Anaphylactic shock It is a severe allergic reaction that occurs as acute cardiovascular and adrenal insufficiency. The basic principles of treatment are similar to those stated above, but in this case, repeated administration of corticosteroid hormones, antihistamines, adrenaline and its derivatives, and heparin should be added. In case of edematous syndrome, dehydration therapy is carried out.
| ← ENCOPRESS | VARIANTS OF JAUNDICE IN CHILDREN → |
|---|
